Navigating Healthcare as an Individual

Introduction
You and I can imagine healthcare intricately tailored to each individual’s genetics, lifestyle, and environment. This vision remains distantly aspirational in today's medical practice of broad, population-based solutions. The bridging of this gap between ideal personalized healthcare and the generalized nature of current treatments is the chasm we must cross to get to the healthcare we all want for ourselves and our families.

The Myth of the Average Patient
Medical research predominantly targets the "average" person, this then forms the basis for many population-based clinical guidelines. Consider the following:
- You may be nothing like the average person.
- You may be nothing like the average person in the study. Your race, your sex, your age group may not be represented in the study that carries the weight of evidence for your recommendation.
- You may be nothing like the size of the person in the study, but note that often the dose applied is exactly the same. Does the size of the dose matter in proportion to your size?
- You may be exactly like a person in the study who did not have a positive outcome.
- It can also be the case that there are studies done whose conclusions suggested that the treatment or drug had NO meaningful impact. It is highly ordinary that those studies simply go unpublished and the one that did show a positive impact was simply the best of the many, further eroding the probability that your treatment advice is likely to work generally, to say nothing for how it may work for you.
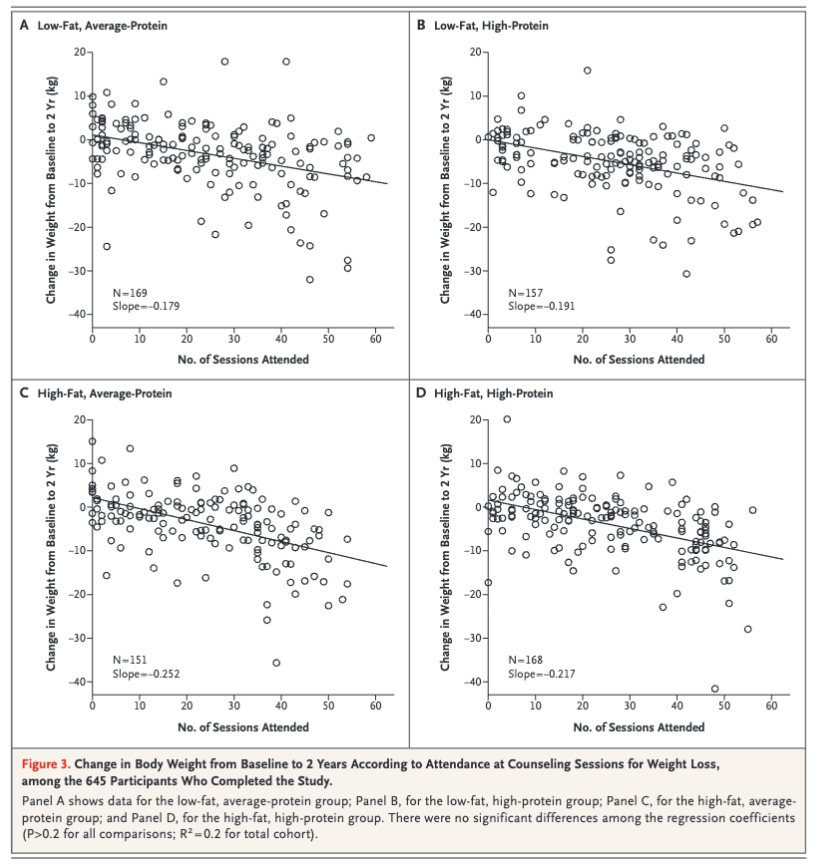
- Consider NEJM Comparison of Diets with Different Compositions of Fat, Protein, and Carbohydrates. The primary conclusion is the composition of macronutrients didn't matter for weight loss. But look at the number of data points above 0, this means that some portion of the measured group, despite going through regular coaching not only did not lose but gained weight. What are the characteristics of those individuals? This phenomenon would exist in most studies and there is a non-zero probability that you are more like those individuals than the average. When that is the case population based medicine may result in an outcome "worse" for you than the treatment.
Variability in Clinical Practice
All this assumes you are lucky enough to get evidence-based guidelines in your engagement. Consider this: you seek opinions from three different clinicians for the same health issue. Are you likely to get the exact recommendations each time? If not, which is right? If 3 are different, logically at least two of them are not the best care possible. Intuitively, if not experientially, we know that this happens.
The Challenge of 'Practicing' Medicine
The term 'practicing medicine' suggests a trial-and-error approach, something like an athlete improving through repeated practice. However, unlike in sports, where results are immediately evident, oftentimes medical outcomes can remain obscure. Patients may not return for follow-up, depriving clinicians of crucial feedback on the effectiveness of their interventions. This lack of outcome visibility impedes the learning process that defines practice, leading to a void of conclusive data on treatment success.
The Risks of Disengagement
Complicating it further, you can't simply ignore the medical system and go fully outside. If you ever have any doubt, pick up a copy of the USMLE. It contains the content a physician is tested on to become a doctor. There are a devastatingly high number of things that can go wrong and desperately require professionals that have dedicated their lives to understanding how to care for patients in life-threatening & painful situations.
But what & how do you actually decide?
Strategies for Empowered Health Decisions
First: understand that you are the decision maker for your own health. It doesn't matter if you feel qualified or not, you will pay the price in the lived experience of your health outcomes. You will pay the price increasingly so from your wallet. The core truth is that everyone else is just advising you.
Big decisions like this demand a process. Following a process will develop skill. Developing a skill will help you navigate you and those your care about through this ultimate high-stakes game. Here are 5 critical ingredients:
- Analyze the Data: Immerse yourself into the underlying studies that inform your treatment. Request access to raw data and analyze the relevance and implications for your specific condition. Be an informed patient & humble about your limits.
- Get Curious with Providers: Explore the evidence base behind your clinician’s recommendations. How well do the study participants resemble you? What were the outcomes for individuals with profiles similar to yours? How variant are your treatment recommendations likely to be?
- Always Tell me the Odds: Consider each medical decision as a calculated risk. Assess the probability of success, weighing it against potential risks and benefits. Is there a 1 in 100 chance of getting a positive outcome? 1 in 20? What are the odds of a negative outcome?
- Get a 2nd Opinion: Solicit alternative perspectives to ensure comprehensive understanding and explore all possible treatment avenues. How variant are the actual recommendations? What are your odds if you do nothing?
- Always Understand the Incentives: Be aware of potential financial motivations that might influence medical recommendations. More commonly this is not driven by ill-intent but an abundance of caution. Knowing the odds means you can make an informed decision for yourself. What are the odds of that knee replacement accomplishing exactly what you hope? What are the odds of things being worse than before? For the price you pay is it worth it for you?
Conclusion: Elevating Patient Agency in Healthcare
My immediate, pragmatic aspiration for healthcare is one of simply informed consent.
Imagine hearing this from the advisors on your medical decisions:
- There are no good studies on XYZ & therefore you likely have something like 1/1000 chance of achieving beyond the placebo effect.
- The studies that were done on ABC did not include people of your race, sex or age & therefore your odds of a good outcome are 1/6 instead of 2/3.
- This drug for your condition has had a blockbuster trial but only extended lifespan for 2 months even in the most positive outcome.
- This treatment costs multiple 5 figures & research suggests a 1 in 2 chance of having a positive outcome and conversely a similar 1 in 2 chance of having an extremely negative outcome.
- Yes, this medication absolutely works in 4/5 patients to improve the surrogate end point of X, but that measurement only translates to a 1/50 chance of reducing mortality risk.
Of course patients will vary in their interest with many choosing to outsource the decision completely to a provider. But too often patients assume:
- probabilities of success are much higher,
- possibilities of negative outcomes are much lower and
- recommendations are much more founded and certain than they really are.
To navigate effectively through the maze of our healthcare system, we need to increase our sophistication as patients and move passive healthcare consumption to active, informed participation. By embracing a role as a critical and questioning participant in our healthcare, we can approach a better state of informed consent in our own healthcare and understand we are the ultimate decision-makers for our own health.