Changing Healthcare?

"We are going to change healthcare!"
"Disruption!"
"Innovation!"
These feel great to say & imagining a better future alone makes you feel better about the state of healthcare. However, there is real, gritty work required to actually make a difference.
The truth is that when we say, "change healthcare" it means "We know & want it to get better!" - but that's all we want to say. Change it to what? How are you going to change it for the better (change can make things worse too!). Do we really know how & why things are the way they are? Chesterton's Fence is a tough one in healthcare since there is so much legacy "fence" there.
The solution is not to give up or be resigned to the status quo, the solution is to get very pragmatic about what it means to make progress.
Defining the Problem
Imagine a patient arrives at a medical facility, she shares her symptoms & a treatment is launched. What are the chances that her treatment would be the same at hospital A vs hospital B? What about hospital A in the morning vs hospital A in the evening? In less critical situations it might not matter that much (although it might). In more critical situations that risk of variation starts to grow.
Think about it this way. Even if there were only 3 ways to receive care for whatever you needed treatment for, if that care is different each time, it means you only have a 1 in 3 chance (at best) of getting the best care. The reality is that any human-led activity will have much more variation than 3 & would include scenarios that could leave you worse than what you started with.
So, the problem: if the treatment varies there is no way for every patient to receive the best care.
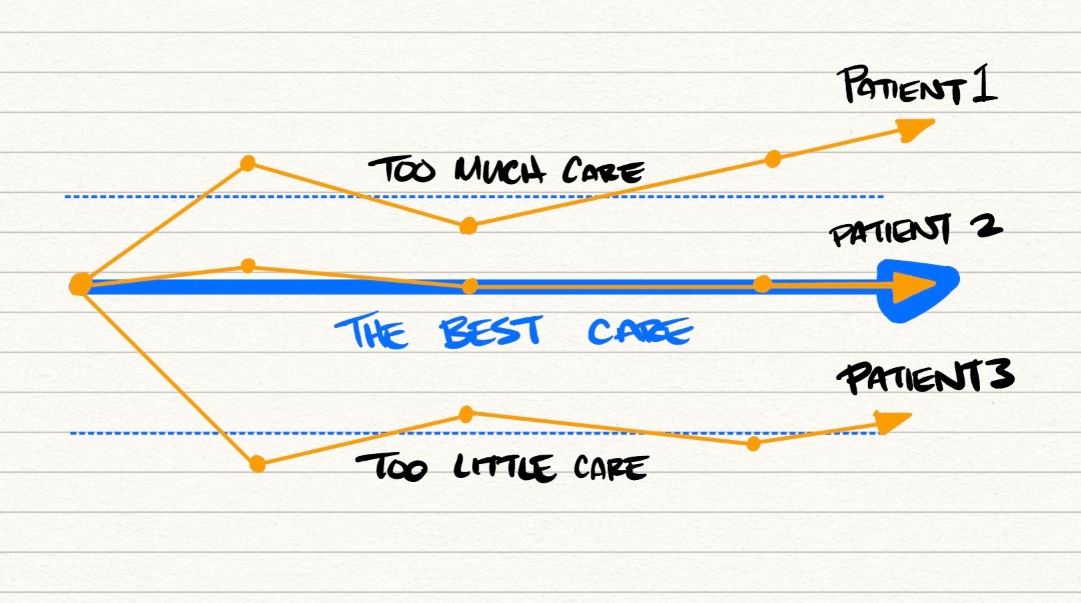
Changing healthcare = changing processes.
The solution to variation & providing the best care to every patient is to use process.
In the 80's and 90's Lean Manufacturing swept through the auto industry, through retail & through seemingly everywhere but healthcare. Though I love the labels, everything from: Gemba & Kaizen to Muda & Andon, the truth is sometimes they just add complexity to simple ideas. Here is how we pragmatically change the way we deliver healthcare by using process:
- Should we do something?
- What is the best process to follow?
- How do we follow the process?
- How well did the process work?
- How do we improve the process?
Let's break it down.
Should we do something?
The first step in a process is to determine whether to do anything at all.
We have all seen the stats. $1T in waste happens in the US Healthcare system. Poorest outcomes per dollar of spending in the world. See here. here. and here.
If the incentives are not right, the system will reward doing something vs doing nothing (even when nothing is better) and ultimately, we will get what we pay for.
The failure to take on risk (Value Based Care, Risk sharing, etc.) then leaves you with the soul-scraping scenario where you can't really look at certain improvement activities because you know you'll be faced with a "Sophie's choice" of deciding between the $ needed to save the mission of your organization and following the best process of care for patients.
So how do you start from where you are? Go at risk. If it is untenable, get ready to go at risk. If you are at risk, start with key processes & clinical guidelines for patients you are at risk with. As your organization's capability at deciding which level of care is best (including when the answer to "Should we?" is no) you can move with more confidence to explore the economic & clinical value that comes from growing the number of patients you have under these care arrangements.
Risk?
You collect or share the premium that is used to pay for care. This can be programs like MSSP/Next Gen or partnerships with payers to take care of patients with a defined budget. Conceptually, think of it like you get $5000 per person you agree to care for and you keep what you don't spend on their care (while hitting quality measurements so you are not rewarded for doing nothing when you should do something.).
What is the best process to follow?
CPMs or Care Process Models are clinical guidelines on how to care for a patient through a particular episode of care. For example, what are the ideal steps that a patient with Sepsis should be taken through? A stroke patient? AMI?
Because change is difficult, the path of least resistance is to take the average of how care is done in your system and follow that. But you don't want the most average care, you want the best.
Similarly, as per problem definition above, reducing variation is the goal - but you want to reduce that variation on the best practice.
You can look externally for best care processes, or you can develop from the best care happening in your organization to start as you improve process by process.
How do we follow the process?
This is more difficult than it seems & is a job yearning for technology to help. [1]
Right data. What data do you need? Where do you get it? Does it exist in the EMR? Is it somewhere else? To follow best practice, you are going to need data.
Right people. Healthcare workers are in a "click-ing" nightmare. How do you get that data to the right people and only the right people. Which roles are part of the process? How do you make that process flexible when roles change or are short staffed?
Right time. If you get the last two right and get this one wrong, you only increase the nightmare. When should a piece of data arrive? How do you get it in real-time? How do you avoid those tasks piling up like your Gmail account to the point of ignorance?
How well did the process work?
Did you actually follow the process? How did it vary from the standard? Why did it vary? Should it have varied? If it went well, why did it? What are we measuring? Do we need to measure new things to help us improve? Find the root cause (RCA) and keep asking why.
RCA
Root Cause Analysis, ask "Why?" 5x.
e.g. 1- Why didn't we follow the process? We forgot. 2- Why did we forget? The urgency of situation meant old patterns took over. 3- Why didn't the urgency trigger the new process? It was not top of mind. 4- Why wasn't it top of mind. The training was too long ago. 5 - why was the training too long ago. We underinvested in the work required to truly teach us to change. Ah, root cause: let's increase training.
How do we improve the process?
After learning, we need to act: How do we add a new person to the process? A new step? How can we quickly adapt the process to account for things that happen at our clinics & facilities? What measurements or data do we need to add to determine how well something is really working?
Not complex enough?
Does this sound too simple? Sometimes the sophistication of terms adds a mystique that makes the knowledge feel more rare and valuable. If so, you can use terms like: 6 sigma, DMAIC, Genchi Genbutsu, or any other that will facilitate application.
Process, Variation & Changing Healthcare
Eliminating unwarranted variation in care from the best possible clinical practice is solved by using and adopting process. It is battle-tested in other industries, malleable and applicable to our needs in healthcare. This is as easy and as difficult as it sounds, but this is what it means to pragmatically "Change Healthcare." Will it happen? It is up to us.